قیمت سوپرفود NBS در سایت دکتر خلخالی | اكسيرشاپ
آرشیو مقالات
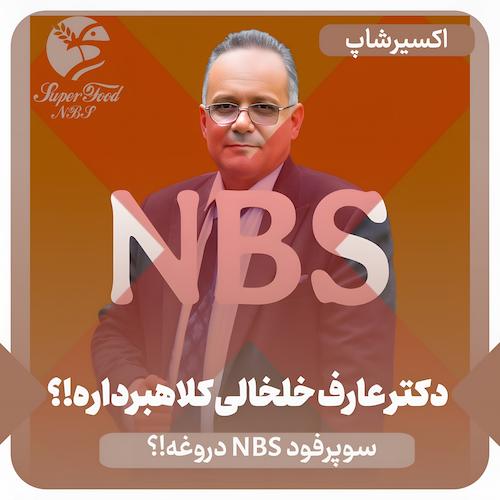
⚠️دکتر عارف خلخالی کلاهبرداره‼️NBS یک دروغه⁉️
چرا این روزها در فضای مجازی بارها میشنویم که «دکتر عارف خلخالی کلاهبردار است» ...
-(1).jpeg)
سوپرفود NBS چیست؟ | راز ترکیبات سوپرفود فاش شد!
بیش از ۵۰ هزار نفر در سراسر جهان از سوپرفود NBS به عنوان بخشی از سبک زندگی سالم...
.jpeg)
پودر سوپرفود NBS برای چی خوبه؟ جواب های شوکه کننده
با وجود اینهمه تبلیغات درباره مکملهای گیاهی، طبیعیست که بپرسیم آیا واقعاً پو...
.jpeg)
طرز تهیه سوپرفود NBS در خانه + تمام نکات
آیا میتوان سوپرفود را در خانه تهیه کرد؟ ایده ساخت یک مکمل مغذی و طبیعی در خانه...

بهترین روغن ها برای درمان زانو درد + بررسی و مقایسه روغن ها
آیا میدانستید تقریباً یکچهارم بزرگسالان از درد زانو رنج میبرند و شیوع آن در ...

معجزهای برای درمان یبوست؛ روشی که ۷۰۰۰ نفر از آن نتیجه گرفتهاند!
آیامعجزه ای برای درمان یبوست وجود دارد؟ قطعاً با علل و علائم یبوست آشنایی دارید...
.jpeg)
مضرات پودر NBS و موارد منع مصرف + تحلیل بی طرفانه
در سالهای اخیر، پودر NBS با عنوان «سوپرفود معجزه قرن» توسط بسیاری از کاربران،...
درمان قطعی کولیت روده با طب سنتی | 100 درصد و تضمینی
فکر میکنید از هر ۱۰۰ هزار ایرانی چند نفر با بیماری دردناک کولیت روده درگیر هست...
مضرات عسل برای زخم معده | جایگزین ها + نکات مهم
آیا عسل که بهعنوان یک خوراکی طبیعی و پرخاصیت شناخته میشود، میتواند برای همه ...

درمان سریع معده درد با عسل | درمان قطعی و طبیعی
🤔 آیا میدانستید یک ماده طبیعی مثل عسل میتواند در کمتر از چند دقیقه به آرام ش...

داروی گیاهی برای معده درد | بدون بازگشت و دائمی
آیا میدانستید بیش از ۳۰٪ افراد در جهان هر سال یکبار معدهدرد شدید را تجربه می...
درمان زخم معده با عسل | معجزه درمان زخم معده!
آیا میدانستید عسل میتواند بیش از یک شیرینکننده طبیعی باشد و حتی در بهبود زخم...